Despite an increased understanding of Parkinson’s disease (PD) and how to treat it, there is still much to be done to help improve outcomes for patients. An interactive session held at the 9th Congress of the European Academy of Neurology, Budapest, July 1−4 2023, looked at different aspects of PD management, including discussions with experts on practical advice for the management of difficult to treat Parkinson’s disease and atypical parkinsonian symptoms.1
Some motor and non-motor symptoms in Parkinson’s disease (PD) are particularly difficult to treat, such as hypokinetic dysarthria, freezing of gait problems, falls, sleep disturbances, cognitive problems and pain.2 Potential management techniques for these symptoms, which could make a difference to improve daily life for patients living with PD, were presented during the session.
Speech and swallowing
Elina Tripoliti, Honorary Associate Professor at UCL, London discussed how to identify and manage speech and swallowing problems in PD. Speech in patients living with PD can vary because of fatigue, presence of saliva/mucosa, posture, medical treatment and stage of disease, but has been shown to be a problem in up to 89% of people with PD.1,3
Speech has shown to be a problem in nearly 90% of people living with Parkinson’s disease3
One of the challenges is a reduced awareness of soft voice, so a patient’s perception of how loudly they talk does not match what others hear.1,4 Intensive voice training such as LSVT LOUD (Lee Silverman Voice Treatment) has been shown to be effective, showing that treatment which targets voice may be uniquely beneficial in improving speech production in PD.3
Swallowing can impact the ability to take oral medication, and a study with patients living with PD found that bigger capsules were easier to swallow than small tablets, especially if swallowed with cold fizzy drinks as both help to provide sensory feedback to the patient.5,6 Professor Tripoliti’s recommendations included optimizing medication intake and providing individualized swallowing therapy, so that patients can see and understand what happens when they swallow.1
Gait and balance
Ota Gál, a physiotherapist from Charles University and General University Hospital Prague, noted that gait disturbances can be seen early in the disease, and can be used pre-clinically to aid diagnosis.7 Issues with balance can also be detected in early disease.8
Studies have shown that as PD progresses, all gait variables deteriorate and freezing of gait (FoG) increases.9,10 Balance also worsens as PD progresses and cognition worsens, leading to an increase in falls. A meta-analysis across 6 PD studies showed a 3-month fall-rate in 46% of participants.11
46% of patients fell during a 3-month period11
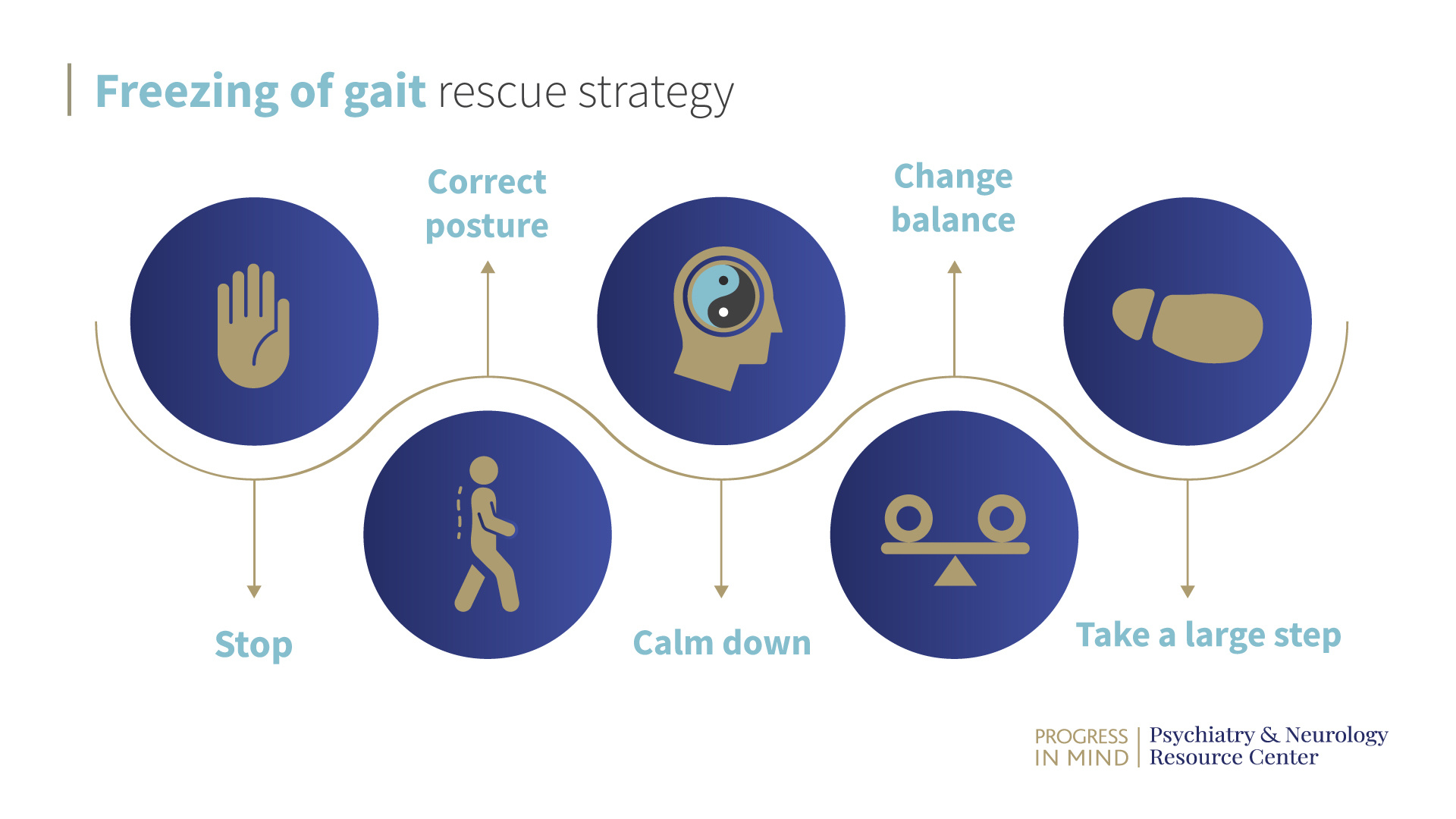
L-dopa has been shown to improve gait, but its effect reduces over time.12 To compensate for this, Ota Gál uses a number of different strategies to address FoG:1
-
Develop a rescue strategy with the patient
-
Increase gait by training on a treadmill
-
Use visual cues, for example stripes and squares on flooring within the house
-
Improve cognitive-motor training, for example with specially developed computer games.
Rescue strategies can be effective for some patients living with PD, but are slow to work through in a real-life setting which can be impractical. Because of this, Ota Gál works with patients to leave out some of the steps and thus reduce the overall time required to complete the strategy. The steps of a rescue strategy include:
A number of studies have shown that exercise, including resistance, aerobic and strength training, can improve balance in people living with PD.13-16 So getting patients to adhere to exercise regimens could have a positive impact on their day-to-day life with PD.
Pain
Pain is a frequent problem for people living with PD, which worsens during the course of the disease and has a severe impact on quality of life.17 Patient education and active management may help alleviate the symptoms, as was discussed in our coverage of other sessions at EAN. Read more in “Highlights from the 9th Congress of the European Academy of Neurology”, here.
PD: Parkinson's disease
UCL: University college London
LSVT LOUD: Lee Silverman Voice Treatment
FoG: Freezing of gait
EAN: European Academy of Neurology
BE-NOTPR-0352, approved: 10-2023