With countries in the OECD* spending around 9% of their GDP** on health systems,1 it is easy to see why it is important to make sure they are truly delivering what the patient needs. To gain insight into how health systems may improve patient care, the recent European Congress of Psychiatry2 assembled a panel of experts to assess the use of patient-reported measures in mental health, including their role in getting a true understanding of what recovery means for each patient and the challenges implementing them in health systems across the globe.
Clinical versus personal recovery
Countries in the OECD spend around 9% of their GDP on health systems1
In the past, clinical recovery in schizophrenia has been defined with full symptom remission, full or part time work, or independent living.3 However, Dr Mike Slade, professor of mental health recovery and social inclusion at the University of Nottingham, disagrees with this definition and has said "he has had to “unlearn almost every level of this understanding,” as it assumes that only patients who have returned to a “normal life” have seen true recovery".
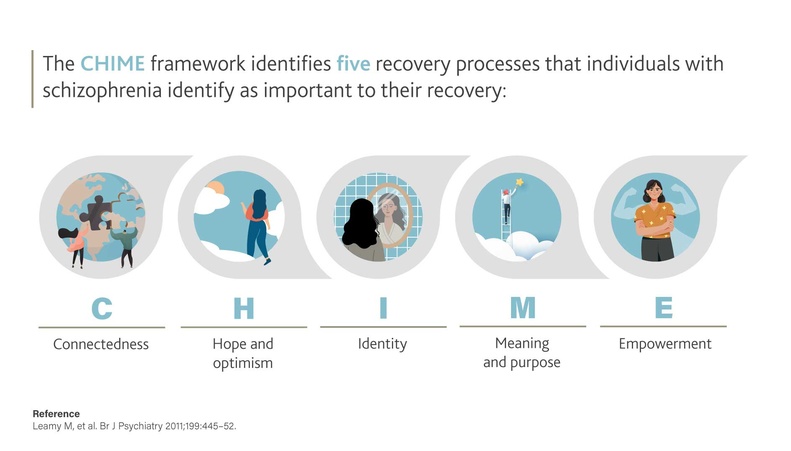
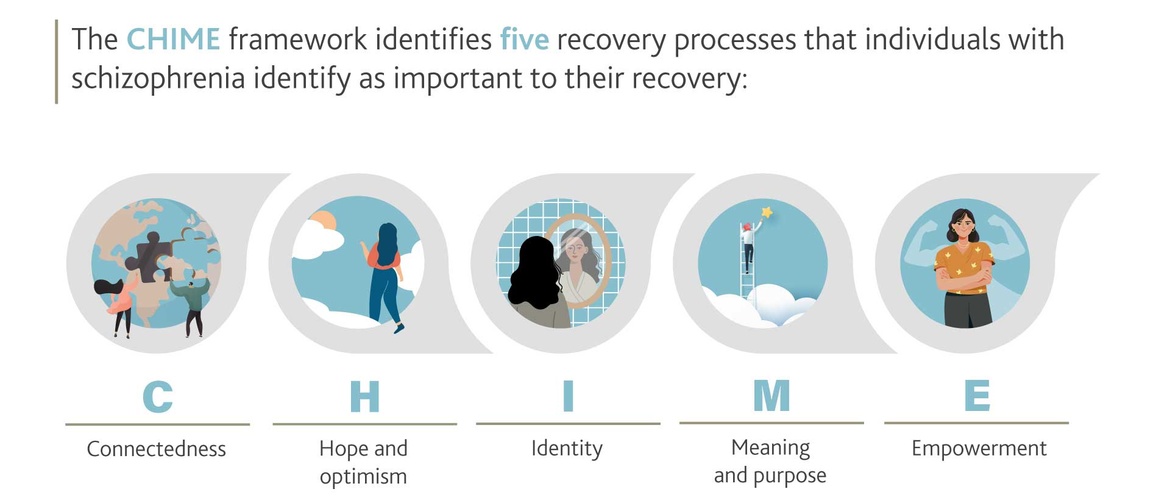
He believes that when we start listening to individuals affected by mental health, they talk about personal recovery – which is why his team developed the CHIME framework.4 The framework was named for the five recovery processes that individuals themselves identify as important to their recovery: Connectedness; Hope and optimism; Identity; Meaning and purpose; Empowerment.
It was noted that in longitudinal studies of patients with schizophrenia, personal recovery was more predictive of outcome than clinical recovery,5 and that personal recovery had a larger impact on patient well-being.6
In patients with schizophrenia, personal recovery was more predictive of outcome than clinical recovery5
Standardizing patient-reported measures
But how do you quantify patient-reported terms, such as “meaning and purpose” or other terms, such as “social inclusion” in a way that provides quantifiable data? This is the question that Katherine de Bienassis, Health Policy Analyst at the Organisation for Economic Co-operation and Development (OECD), is trying to answer.
Patient-reported outcome measures and patient-reported experience measures (PROMs and PREMs) are best placed for this, however, the use of patient-reported measures in mental health care is limited to a small number of countries and settings.7 By harmonizing these tools internationally, more insight may be gathered which can then allow health services to learn and improve, and to deliver the ultimate objective of health care: maximizing people’s health and well-being.7
To reach this end, the PaRIS (Patient-Reported Indicator Surveys) initiative was launched in January 2017. This program aims to develop, pilot and implement new patient-reported indicators in a way that can be standardized in health systems in multiple countries.7
Initially, a panel of experts came together to identify the priority domains of PREMs and PROMs that would be used during the first pilot data collection. All three key areas of PREMs were covered: treatment with respect and dignity; shared decision making; communication and relationship with the healthcare team. Only one area of PROMs was covered: restoration of well-being.7
The use of patient-reported measures in mental health care is limited to a small number of countries. By harmonizing them, more insight may be gathered which can then allow health services to learn and improve7
First data collection results
For the first pilot data collection, 12 countries submitted data overall with a number of sites able to implement new data collections. This served as proof that international benchmarking in this area would be possible – “an exciting step for improving harmonization of PROMs and mental health care.”
The results for one site in particular were discussed in detail at the congress: Elisabetta Scanferla, clinical researcher at Sainte-Anne Hospital in Paris, was able to share how patient-reported measures were implemented in one French public psychiatric hospital. When compared to patient arrival, improvement in the PROMs domain was seen across all indicators at discharge.8
When compared to patient arrival, improvement in the PROMs domain was seen across all indicators at discharge8
On average, the increases were between 10% and 15%, which were found to be similar with other countries participating in the PaRIS program, namely Belgium, Japan and Portugal.7,8 This is a significant change as assessments have shown that, on average, a 10% increase is seen upon finding employment,9 showing the importance of intervention and treatment.
In the PREMs domain, high satisfaction was reported across all indicators although the worst results were seen in time spent by the clinician and involvement of the patient in care,8 potentially serving as an indicator that could guide clinicians to improvements in their daily practice. Elisabtta Scanferla also found that although there was significant correlation between subjective well-being PROMs and PREMs, the PREMs results could not be used as a way of predicting PROMs.8
Although there was significant correlation between subjective well-being PROMs and PREMs, the PREMs results could not be used as a way of predicting PROMs8
Challenges of implementing PROMs and PREMs
Although the first data collection of the PaRIS initiative has shown positive results, there are still limitations and challenges that come with implementing PROMs and PREMs into health systems. In this study, only one primary domain of PROMs was utilized, indicating that more development is needed at the international level when relating to PROMs in mental health care.
Furthermore, Elisabetta Scanferla believes that the costs and burdens that come with data collection will only increase with the lack of integration of PROMs in clinical practice. One often overlooked challenge is accurately translating these surveys into multiple languages, which according to Dr Bernd Puschner, senior researcher at Ulm University’s Department of Psychiatry, might even take more work than collecting and analysing the data itself.10
Personal recovery demonstrated its value in predicting outcomes and international benchmarking was proved possible5-7
Overall, the PaRIS initiative has been seen as a success by the members of the OECD, with a second data collection set to launch in 2023.2 One aim of the second data collection is to standardize the data collection of PROMs in different medical disorders to address the fact only one PROM domain was included in the pilot. However, with personal recovery demonstrating its value in predicting outcomes5,6 and proof that international benchmarking is possible7, an exciting step has been taken for PROMs and mental health care.
*Organisation for Economic Co-operation and Development
**Gross domestic product
CHIME : connectedness, hope and optimism, identity, meaning and purpose, empowerment
OECD : Organisation for Economic Co-operation and Development
GDP : gross domestic product
PROMs : Patient-reported outcome measures
PREMs : Patient-reported experience measures
PaRIS : Patient-Reported Indicator Surveys
BE-NOTPR-0316 approval date 06/3023